What FODMAP is gluten?
Starting a low FODMAP diet, and working out which food to eat can be a daunting task. In our next couple of blogs, we want to address some of the frequently-asked questions from people new to the diet.
One of the most common FODMAP-related Google searches is “What FODMAP is gluten?”. The answer is that gluten and FODMAPs are two different things, but they are both found in wheat, which is why there is often confusion between the two.
Read on to find out about the differences between gluten and FODMAPs. How the two can affect people with gut issues, and what dietary changes you may need to make depending on your particular condition. - And the good news is that there are options for everybody 😀
Gluten versus FODMAPs
Gluten is a protein found in wheat, barley, and rye. It is not a FODMAP. Gluten causes an auto-immune response in people with coeliac disease. For people with coeliac disease, even small amounts of gluten can damage the lining of the small intestine.
FODMAPs, on the other hand, are short-chain carbohydrates that ferment in the gut, leading to gut symptoms in people with IBS due to something called visceral hypersensitivity. Wheat contains several FODMAPs:
·Fructans: These are the most common FODMAPs found in wheat.
GOS (Galacto-oligosaccharides): These are another type of carbohydrate found in wheat that can cause digestive issues in some people
·Fructose: This is a simple sugar found in found in wheat. Fructose can cause digestive issues, but it is usually at way too small a concentration in wheat products to be a problem
What to look out for
If you’re following a low FODMAP diet, choosing products or restaurant dishes labelled “gluten-free” can be a quick way to find suitable options that are free of wheat.
However, it’s important to note that not all gluten-free products are low in FODMAPs. Some gluten-free products may still contain high FODMAP ingredients, such as honey or high fructose corn syrup.
In your local pizzeria, a gluten-free pizza, may have a wheat-free base, but have high FODMAP ingredients in the sauce and toppings like onion, garlic and mushrooms. You’ll need to carefully specify your needs.
In the shops, most of the gluten-free pastas made from rice, quinoa or corn are fine up to a serving size of a cup (cooked), but red-lentil based pasta has only a very small low-FODMAP serving size.
Our hot tip is to slightly undercook gluten-free pasta to stop it going mushy.
Breads containing soy flour may be gluten-free, but still be high in FODMAPs.
Not a solution for everyone
It’s also important to note that not all people with IBS are sensitive to FODMAPs.
The full low-FODMAP diet (or process) has three stages –
1. Elimination – eliminating all moderate and high FODMAP foods for 2-6 weeks
2. Reintroduction - testing FODMAPs through staged food challenges to identify triggers
3. Modification – personalised long-term diet that includes well tolerated foods and only restricts FODMAPs that trigger major gut health symptoms
Read more about it in our beginner’s guide here.
Undertaking the first stage will indicate if FODMAPs trigger your gut symptoms. If you are ready to give that a try, a great place to start is our Good Gut Challenge - with a FREE 10-day meal plan.
Completing stage 2 will help you identify if fructans from wheat are a particular FODMAP group that you need to avoid.
Low-FODMAP, not No-FODMAP
People with coeliac disease have to avoid gluten completely, even taking care to avoid cross contamination from cutting boards, fryers, and toasters..
However, people with IBS should note that the low FODMAP diet is not the no-FODMAP diet. Very few foods are so high in FODMAPs that you have to exclude them completely on the elimination stage of the diet (only garlic, onion and inulin spring to mind). For the majority of foods there is a ‘green’, low FODMAP serving size,
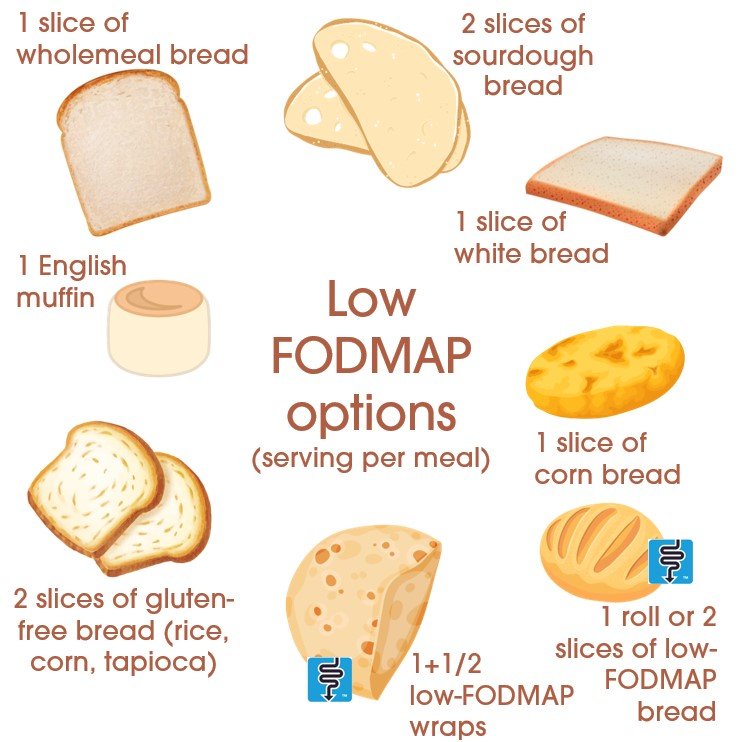
You don’t have to give up bread
Yes, that’s right you have many bread options on the low-FODMAP diet. These are the low FODMAP serving sizes of some breads.
Sourdough (white, wholemeal, spelt): 2 slices
White sliced bread: 1 slice
Wholemeal bread: 1 slice
Gluten-free (white): 2 slices
Corn bread: 1 slice
English muffin: 1 muffin
The long proofing time used to make sourdough reduces the fructan content, so this is a good option to go for.
Steer clear of barley, or pumpernickel and other rye-based breads, these are very high in FODMAPs (and gluten). Similarly, breads made from soy flour might be gluten-free, but they also contain FODMAPs.
Look out for the blue logo
There are several brands that have undertaken FODMAP testing and certification either with Monash University or FODMAP Friendly. Look out in Baker’s Delight, Brumby’s Bakery, and the Pocket Storehouse in Queensland for their special low FODMAP breads. On the supermarket shelves, you’ll find low FODMAP options from Schar and Schnitzer. We like Simson’s Pantry low FODMAP wraps
Baked treats like biscuits are fine in moderation – 1 plain cookie or shortbread is low-FODMAP.
Other options
Swapping out wheat, rye, and barley for other sources of complex carbohydrates will help lower FODMAPs. Potatoes are a great choice for fodmappers and folk with coeliac disease. The following grains have a decent low FODMAP serving size.
Low FODMAP servings of grains (cooked):
Quinoa (red, white or black): 1 cup
Rice (brown or white): up to 500g
Millet: 1 cup
Rice cakes: 4 cakes
Pancakes made with buckwheat flour, are both gluten-free and low-FODMAP. Despite the name, buckwheat isn’t closely related to wheat. It isn’t even a grain.
Low FODMAP breakfast options
When choosing a muesli or breakfast cereal, you’ll likely have to look out for gluten-free options without fruit. Carmen’s have a certified option - our try our recipe here.
Gluten-free Weet-bix is low-FODMAP. Similarly, rice and corn-based cereals like Kellog’s Corn Flakes and Kellog’s Rice Bubbles are low FODMAP. Kellog’s Corn-Flakes Gluten-Free and Special K Gluten-Free are both low FODMAP and suitable for those who have coeliac disease.
Another alternative for a delicious breakfast is a smoothie made with Superflora protein, fibre and probiotics. It is gluten-free and certified low FODMAP by Monash University. It’s great blitzed with lactose-free milk and a low-FODMAP serving of fruit (1/3 of a banana, 1/3 of a cup of raspberries) or some peanut butter. Our favourite smoothie recipes are here.
What about oats?
Oats can be a problem for people with coeliac disease for two reasons:
Oats can be contaminated with wheat, rye or barley that contain gluten and
Oats contain a protein called avenin similar to gluten that can also cause gut inflammation for some coeliacs. Avenin is present at only low levels in oats, but it can cause problems for up to 10% of people with coeliac disease.
Oats also contain a small amount of FODMAPs (fructans and GOS), but there is a substantial low FODMAP serving size for traditional rolled oats, which is 1/2 a cup.
Non-coeliac gluten sensitivity
Mmm this is a tricky one. The existence of non-coeliac gluten sensitivity (NCGS) is controversial. Some studies have indicated that it is FODMAPs rather than gluten that is the problem for this group.
Current evidence suggests that a very small subset of people with IBS may react to gluten, although there is no clear way to diagnose NCGS.
You may want to work with a dietitian, if you’ve tested negative for coeliac disease, but think that it’s gluten not the fodmaps in wheat products that are causing you problems.
Get help
We’ve seen that there are plenty of options, but specialist diets can be complex. If your head is still whirling, and you may want to seek the guidance of a dietitian.
They can help you navigate the later stages of the low FODMAP diet and provide guidance on how to follow the diet safely and effectively.
Good luck!
Written by: Dr Mary Webberley, Chief Scientific Officer at Noisy Guts. Mary has a background in biology, with two degrees from the University of Cambridge and post-doctoral research experience. She spent several years undertaking research into the diagnosis of IBS and IBD. She was the winner of the 2018 CSIRO Breakout Female Scientist Award.