How to master the low fodmap diet, even if you don’t know what a fodmap is.
Ugh! Getting your head around the low fodmap diet can be overwhelming. The FODMAP acronym is convoluted and the science is complex. If no one can pronounce it or understand it, who’s going to try it?
In today’s blog, we’ve put together a beginner’s guide to help you understand the fodmap diet and how it can help your gut health, without needing a PhD in Biochemistry. Rest assured that the team at Noisy Guts all have PhDs and have completed FODMAP training with Monash University, so we’ve got the science covered.
What are fodmaps?
Fodmaps are a collection of fermentable carbohydrate molecules poorly absorbed and digested in people with Irritable Bowel Syndrome and other gut health issues.
Fodmap stands for fermentable oligosaccharides, disaccharides, monosaccharides and polyols.
What does fodmap stand for?
F - fermentable
O - oligosaccharides
D - disaccharides
M - monosaccharides and
P - polyols
The acronym was coined by researchers in 2005 because, at the time, there was no collective term for describing these poorly digested molecules. Imagine what they might be called if they hired a marketing guru?
There are a number of ways in which foods containing fodmaps leads to cramping, bloating, farting, constipation and diarrhea in people with IBS and other gut health issues. To help explain, we’ve translated the science into a 2-minute animated video.
How does a low fodmap diet help IBS?
Isn’t fermentation normal?
Fermentation in the gut is a normal part of the digestive process. But in people with IBS, high fodmap content encourages excess fermentation causing problems.
Fodmaps are either slowly absorbed in the small intestine or not absorbed at all. They attract water into the intestines (result = bloating) and rapidly ferment (result = bloating + farting). And that’s why many IBS sufferers “feel” when trouble is brewing.
Fermentation leads to bubble, bubble, boil and trouble.
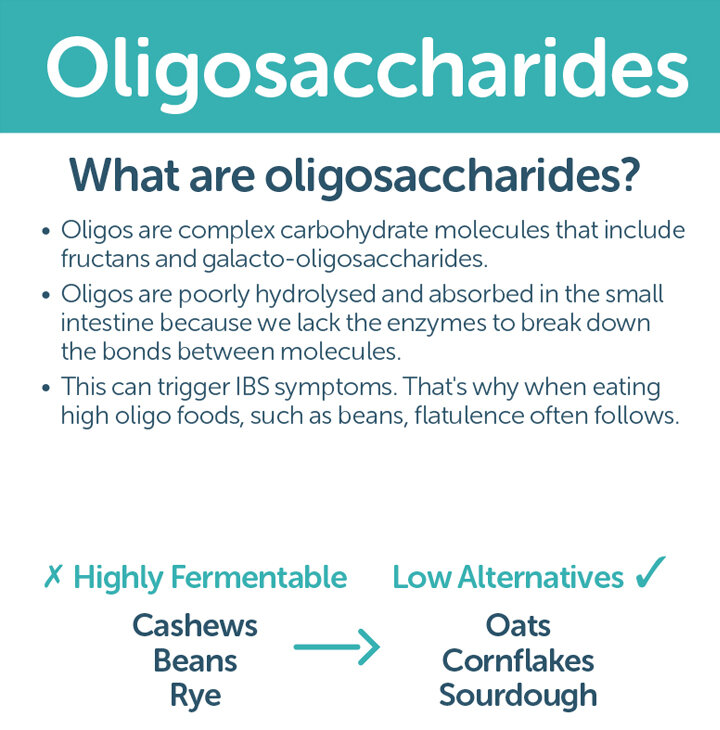
What is an oligosaccharide?
Oligos (Greek word meaning a few sugar molecules) are made up of a number of sugar molecules including fructans and galacto-oligosaccharides. Oligos are hard to digest, with 90% bypassing the small intestine and heading straight to the colon.
Interesting fact: fructans are malabsorbed by everyone because humans lack the enzyme needed to break them down into simple sugars. While smallish amounts of fructans are generally well tolerated by most healthy people, high amounts can cause reflux, farting, bloating and cramping. These symptoms are exacerbated in people with IBS.
Much loved oligos include onions, garlic, leeks and legumes (soya beans, chickpeas and lupin).
What is a disaccharide?
There are three disaccharides – lactose, sucrose and maltose. Lactose malabsorption affects 6% of Aussies, but prevalence varies widely among different ethnic groups.
Lactose malabsorption occurs when the body doesn’t produce enough of the enzyme lactose needed to break down the sugar molecules. Lactose that isn’t absorbed in the small intestine attracts water into the bowel and encourages fermentation to occur in the large intestine. This causes diarrhea, bloating and abdominal cramping.
Foods with high levels of lactose include cows’ milk, soft cheeses, custard, sweetened condensed milk, evaporated milk and ice cream. You can still have your hot chocolate, but you’re going to have to experiment with low lactose milks – the good thing is that there are now lots of options in your local supermarket.
What is a monosaccharide?
Monosaccharides are the sweetest of them all.
Monosaccharides are simple sugars - the most common type is fructose.
In people with IBS, fructose can be malabsorbed, drawing excess water into the gut.
Foods rich in excess fructose include apple, pear, mango, some dried fruits, artichoke, asparagus, honey and fruit juice.
What are polyols?
Polyols are slowly absorbed, but quickly fermented.
There are two polyols to be avoided on the low fodmap diet – sorbitol and mannitol.
These are found in many fruits, vegetables and artificial sweeteners (look out for ingredients ending in ‘ol’).
This explains why your chewing gum may come with a warning that says – excess consumption can have a laxative effect!
How does a fodmap diet work?
The fodmap diet involves a 3-step process of:
1. elimination – eliminating moderate and high fodmap foods for 2-6 weeks
2. reintroduction - testing fodmaps through staged food challenges to identify triggers
3. modification – personalised long-term diet that includes well tolerated foods and only restricts fodmaps that trigger major gut health symptoms
If you can work out which of the fodmaps trigger your gut health symptoms, you can eliminate and/or minimise them from happening.
How to survive on a low fodmap diet
At Noisy Guts, we’ve put together a 5-point plan to survive (and thrive) on a low fodmap diet.
1. Get help! Dr Google is great, but nothing beats a fodmapped trained dietitian. A recent study found that people attempting the low fodmap diet without a dietitian were twice as likely not to achieve satisfactory relief from their IBS symptoms.
If you don’t have a dietitian on hand or not sure who has undergone fodmap training, just email us and we’ll send you a list of trained dietitians in your area.
2. Start with small changes. This is a low fodmap diet, not a NO fodmap diet. So start with simple substitutes such as replacing honey with maple syrup and apples with strawberries. You can find lots of easy switcheroos in our blog. There are two apps that can really help as you make your way around the supermarket: the FODMAP FRIENDLY app and Monash University’s FODMAP app. Both provide lifetime access to databases of fodmap content on fruits, vegetables and other comon foods, as well lists of manufactured products that have passed stringent testing.
3. Don’t forget fibre. Most Aussies simply don’t eat enough fibre. The World Health Organisation recommends 25-30 grams per day for adults. But it’s not just about the quantity of fibre, it’s about the type of fibre that matters. Getting enough fibre can be challenging when you’re following a low fodmap diet. Eat lots of high fibre low fodmap foods such as quinoa, chia, psyllium and kiwi.
4. Make it social. Following a low fodmap diet can make you feel socially isolated, especially during the elimination phase. There’s an amazing group of fodmappers online willing to offer tips, tricks and recipes swaps. And if you’ve not keen on social media and not living in a COVID lockdown, head to your local supermarket and farmer’s markets. You’ll find low fodmap pasta sauces, simmer sauces, stocks and snacks.
5. Get onboard. Following any diet longterm requires a solid support system. Get your household onboard by adapting family favourites and celebrating new recipes. Spend time each week doing meal planning and preparation. You’ll find lots of recipes on our website for inspo. And consider keeping a low fodmap shake on hand for those situations where there are no gut-safe options available.
Want free low fodmap recipes?
Check out our tried and tested low fodmap recipes.